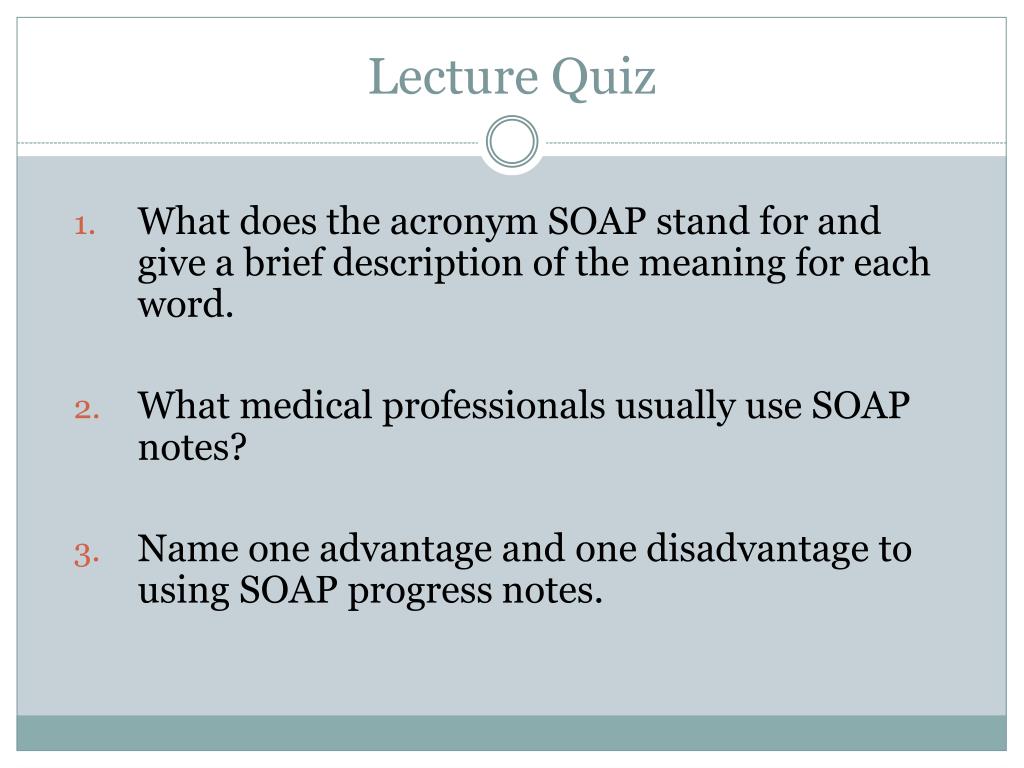
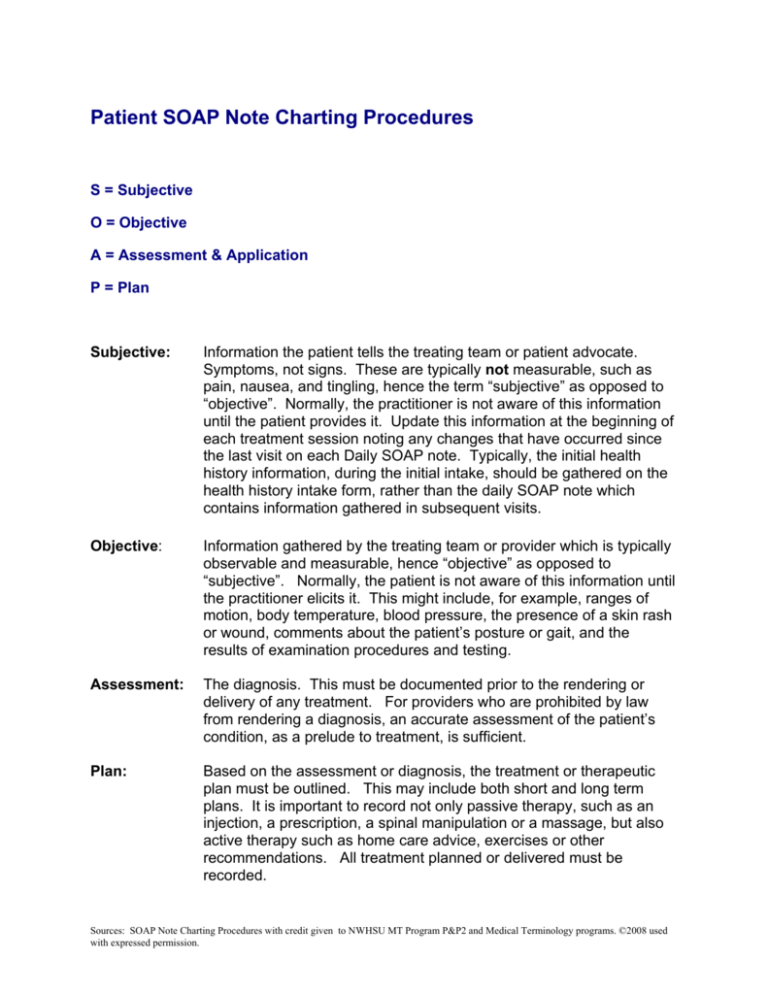
Whether covered by insurance or not, good clinical notes support the rationale for treatment and are necessary should there be a lawsuit or medical issue that requires the patient record be examined The following is an explanation in lay terms as toSOAP Method 30 Minute Devotionals With Meaning SOAP Steps 1 Pray (5 minutes) use a list you have prepared 2 Read your Bible (10 minutes) – have a plan 3 Journal using SOAP method (10 minutes) a S = Scripture Write down a meaningful scripture from your reading bList of 3 best SOAP meaning forms based on popularity Most common SOAP abbreviation full forms updated in June 21

The Evolution Of Office Notes And The Emr The Caps Note Consult Qd
S.o.a.p notes meaning
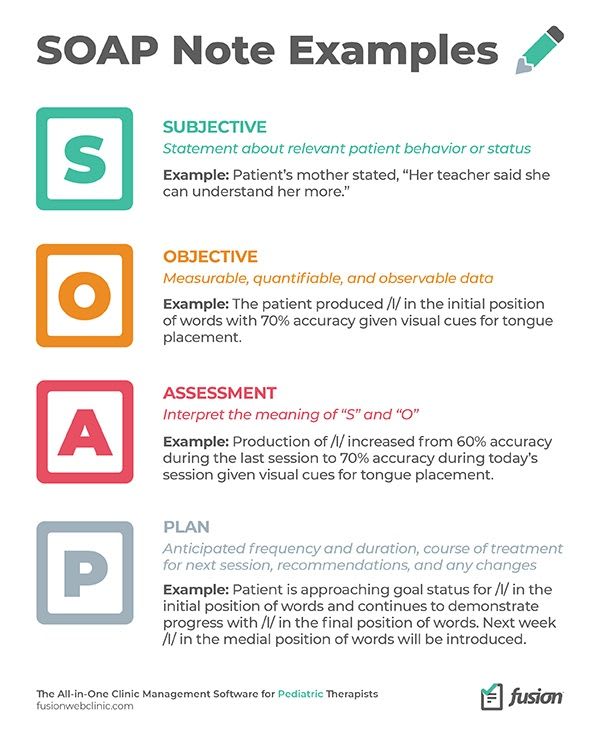
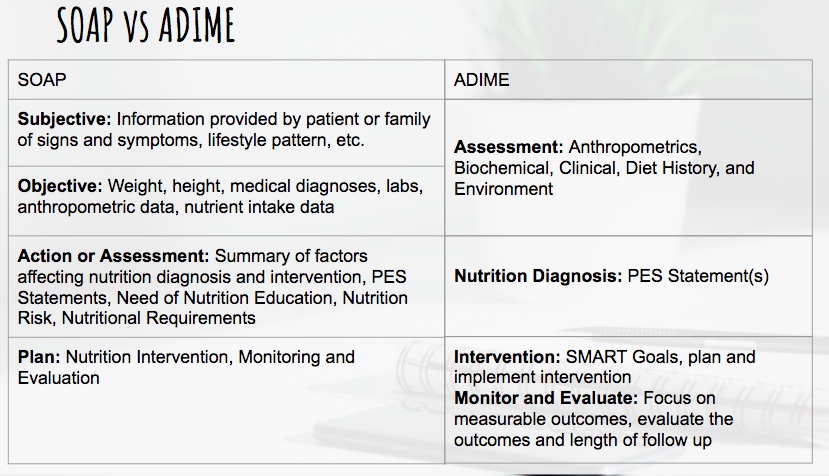
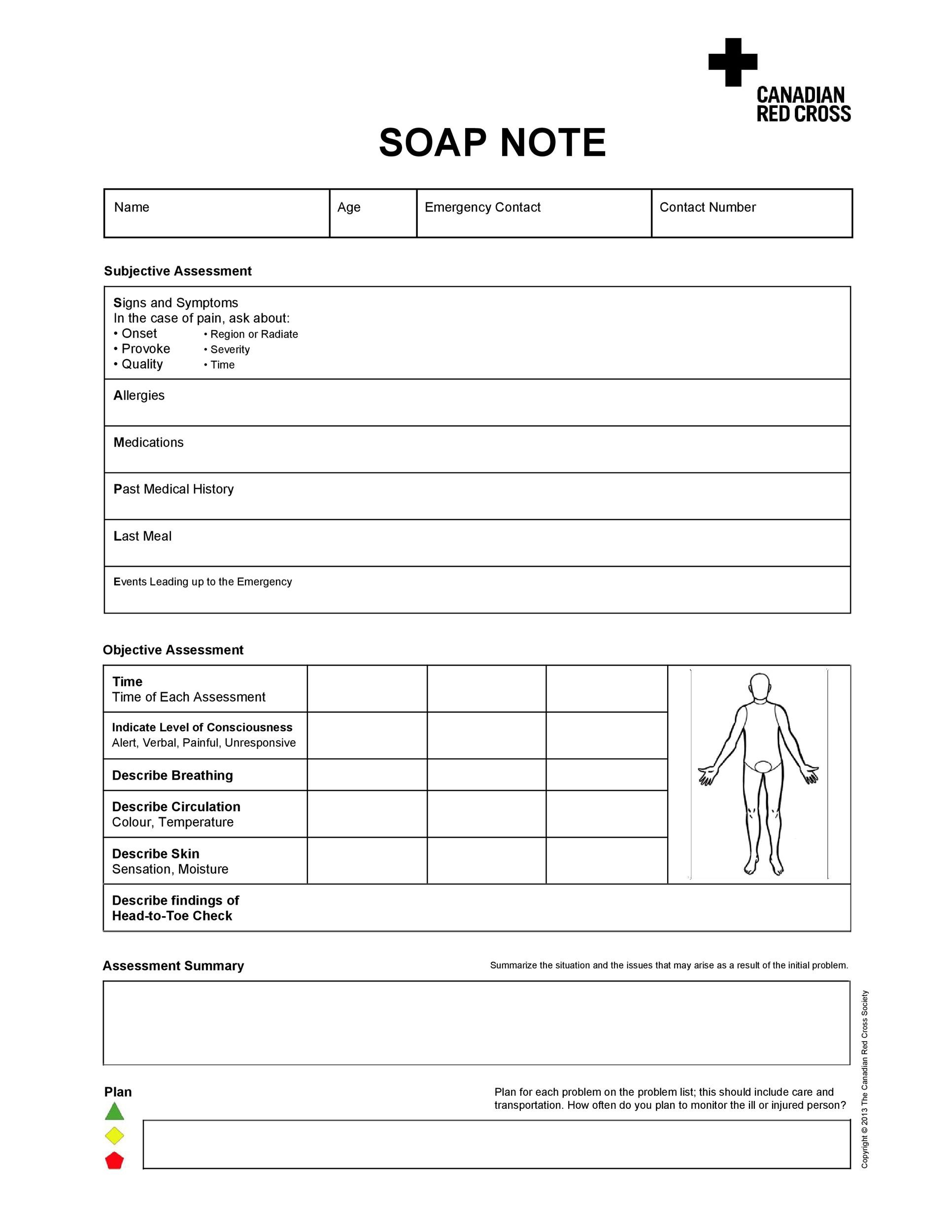
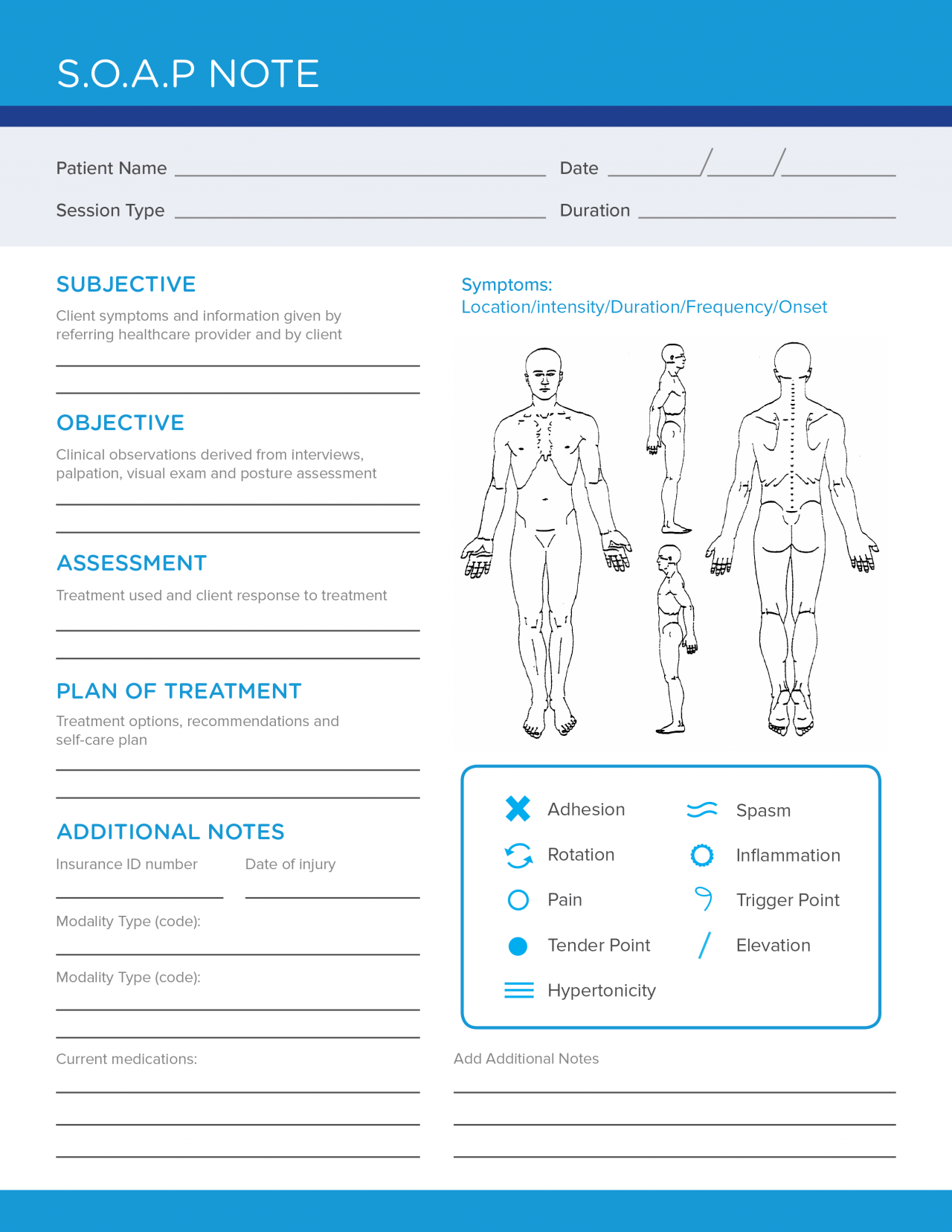
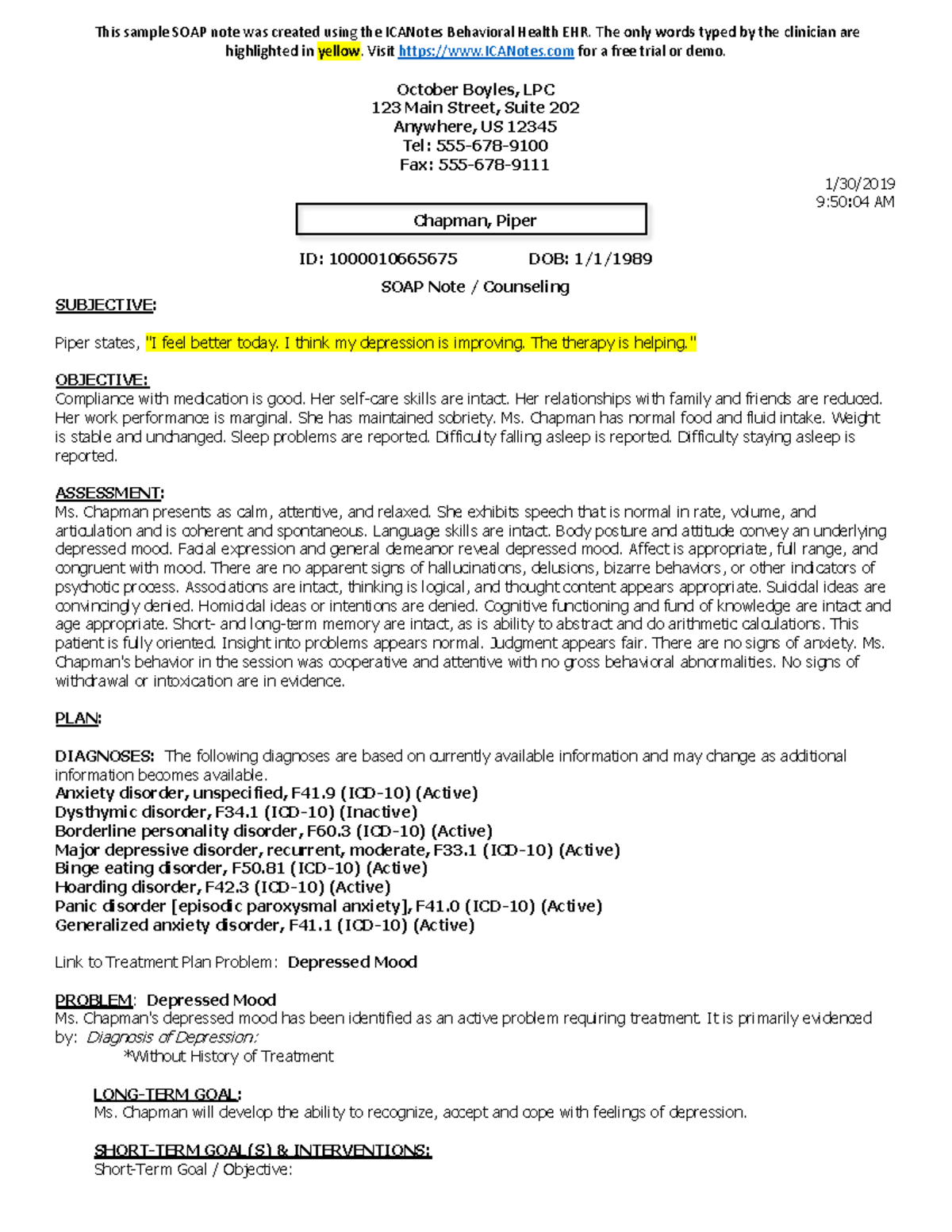
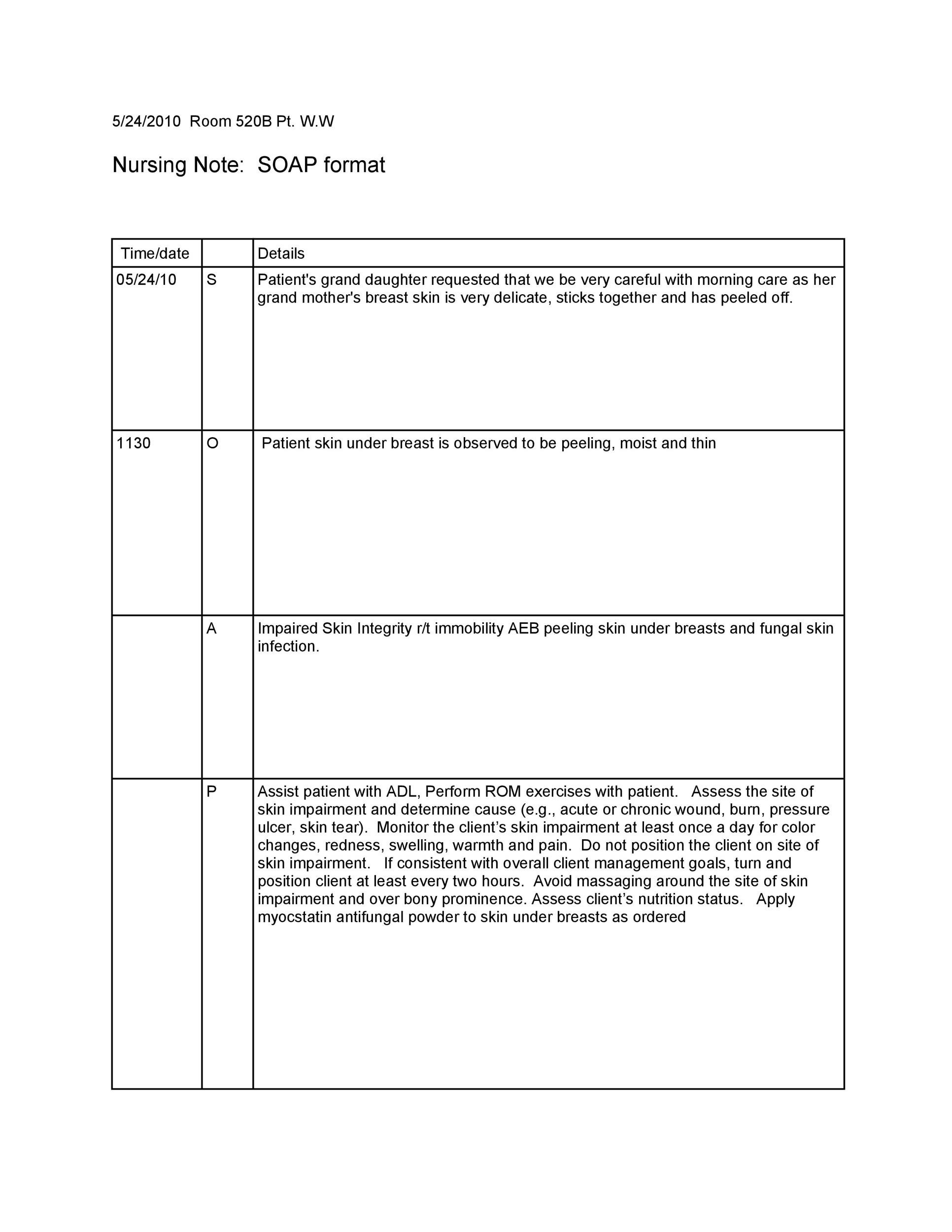
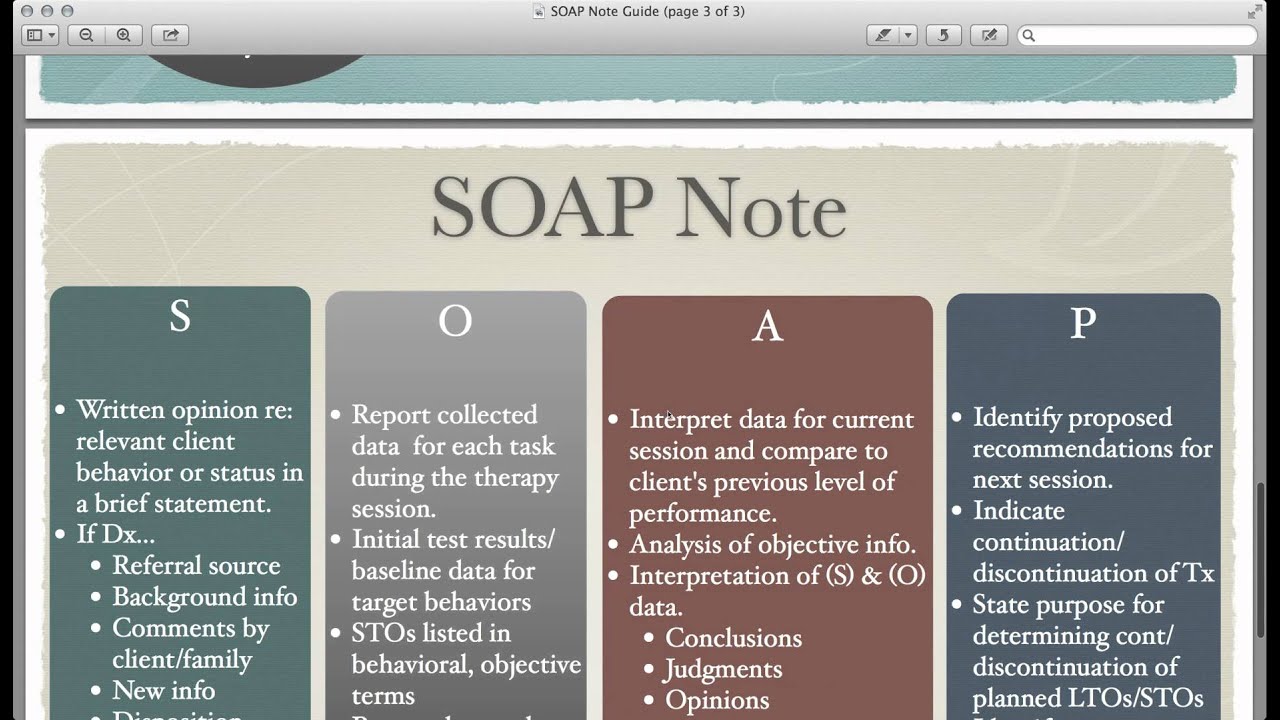
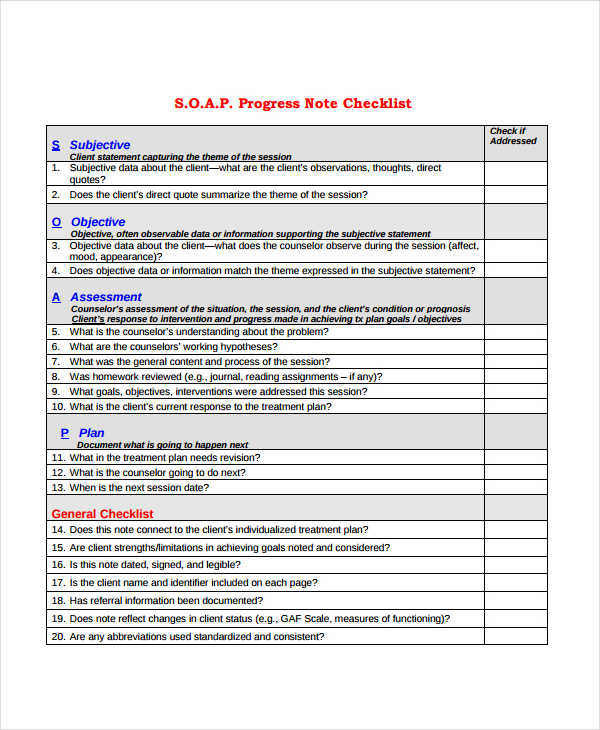
S.o.a.p notes meaning- Some other items a Social Worker should document in their case notes Goal being addressed in session Risk assessment – whether there is any danger to self or others and what the plan for addressing is Date and Time session begins and ends and length of session Progress towards discharge plan The primary thing to keep in mind is that SOAP notes are meant to be detailed, but not lengthy They are a clear and concise record of each interaction with the patient or client Following the format is essential, but it is possible to reorder it so that the assessment and plan appear at the top (APSO)




Free Soap Notes Templates For Busy Healthcare Professionals
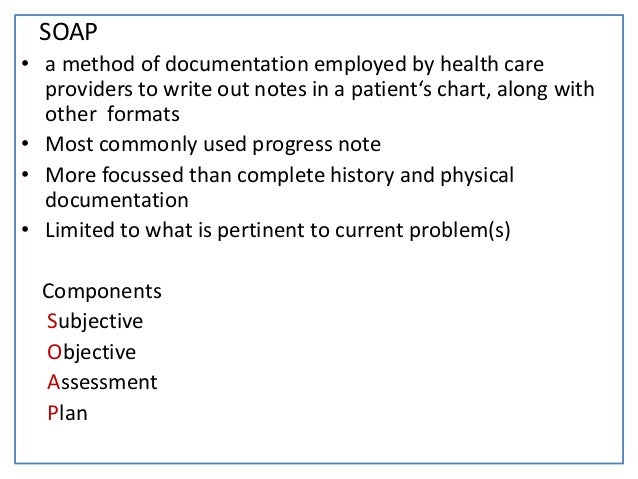
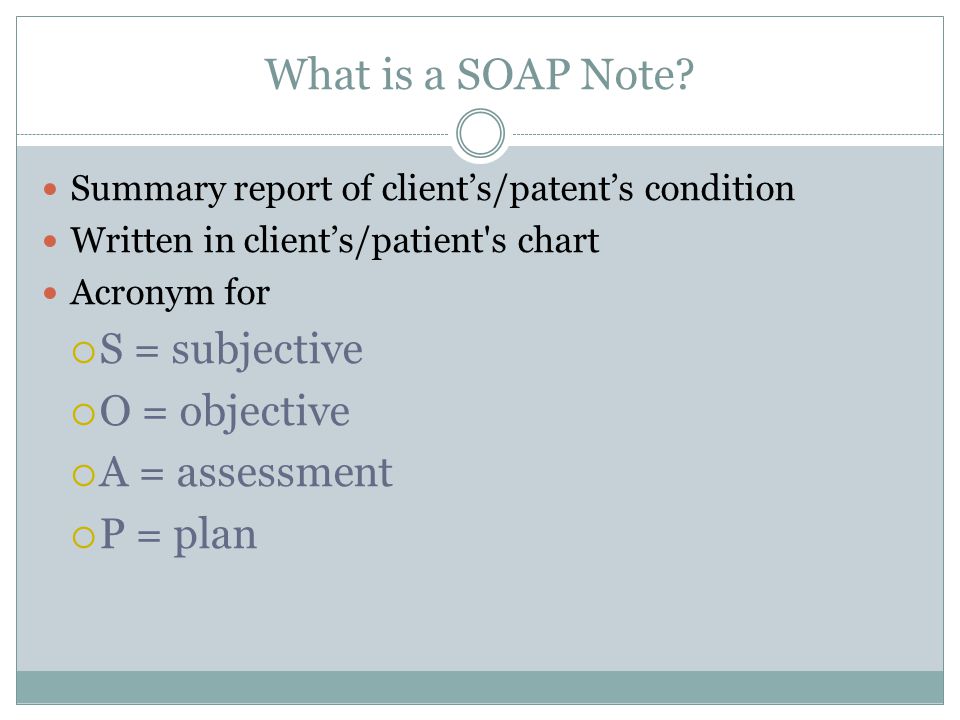
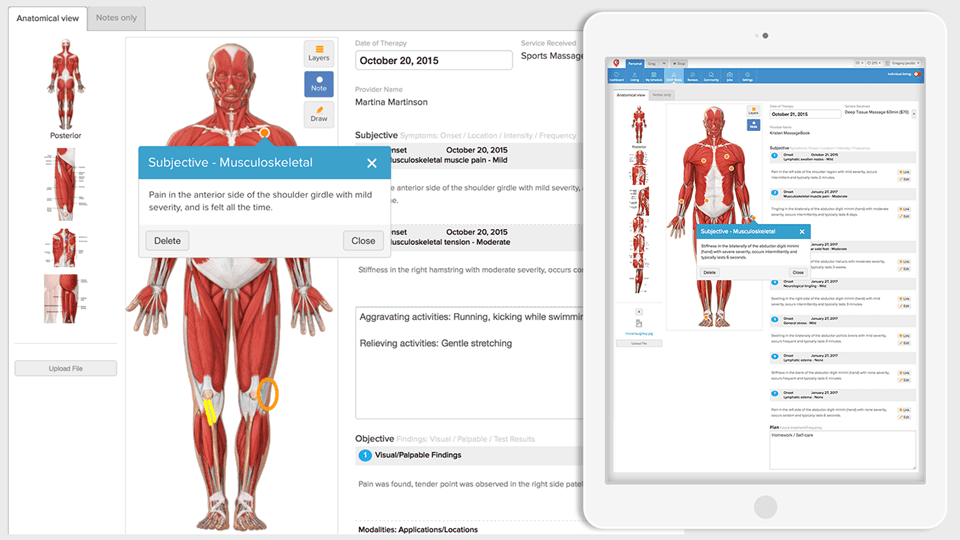
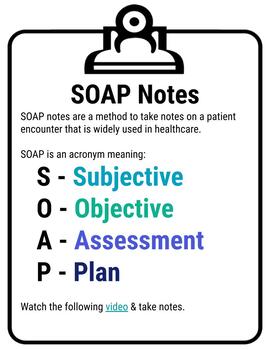
The SOAP note is a way for healthcare workers to document in a structured and organized way This widely adopted structural SOAP note was theorized by Larry Weed almost 50 years ago It reminds clinicians of specific tasks whileSOAP is a method of Bible reading and journaling It can be used with any daily Bible reading plan Open your Bible to today's reading (according to whatever plan you are following) Take time reading and allow God to speak to you When you are done, look for a verse that particularly spoke to you that day, and write it in your journalREAL MASSAGE PHOTOS http//wwwRyanHoymecomLARGEST MASSAGE WEBSITE http//wwwMassageNerdcomhttp//wwwFaceBookcom/massagenerds http//wwwTwittercom/m
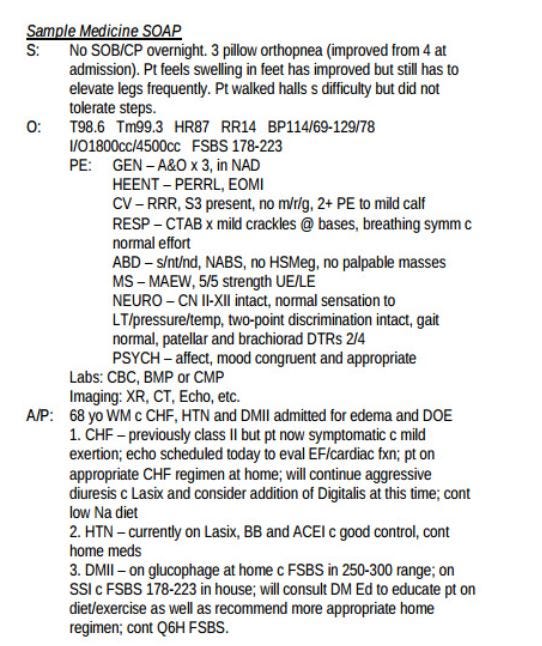
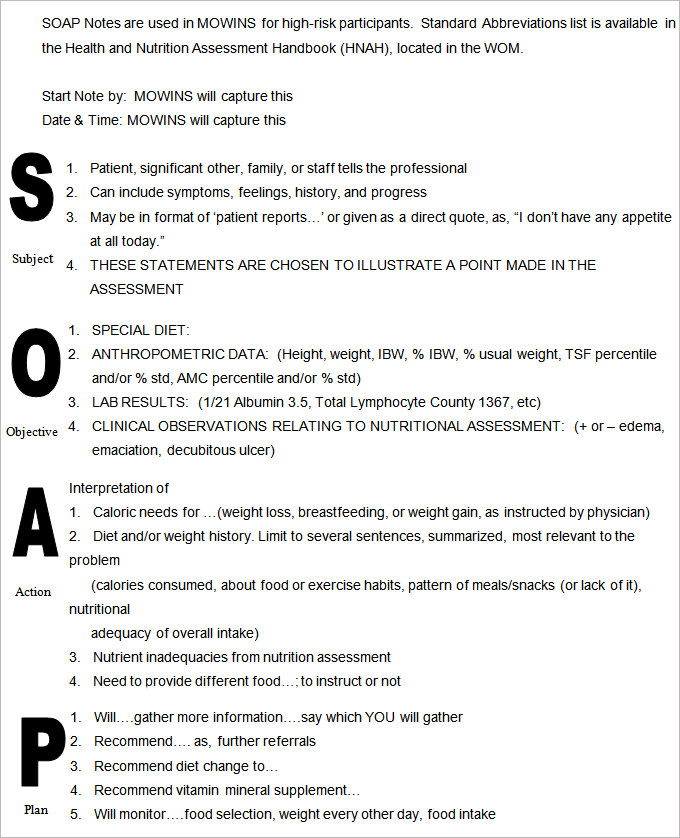
General notes air distribution plan notes north enlarged boiler room plan north mechanical room plan detail 'a' fan coil installation detail 'b' terminal unit hydronic coil piping with 3way valve detail 'c' exterior equipment pad adjacent to building detail 'd' heating water piping schematic The SOAP note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare providers to write out notes in a patient 's chart, along with other common formats, such as the admission note SOAP stands for Scripture, Observation, Application, Prayer It's a great way to delve more deeply into your Bible reading, and record your thoughts, emotions and connections when studying scripture
Brian Dear Leave a comment on DAP vs SOAP Notes for Counselors and Therapists Data, Assessment, Plan These are the fundamental building blocks of the DAP note While they serve the same purpose as a SOAP note, DAP is a slightly different format What you choose is entirely up to personal preferenceO This is where the SOAPS method can really help to begin creating definitive statements that can be used to evaluate the primary document 2) Writing and Proving Inferences A) Using the information collected in the attention getter, have students write aWhat does SOAP abbreviation stand for?



Www Lamar Edu Fine Arts Communication Files Documents Speech Hearing Soap Notes Pdf




Writing Samples
SOAP notes are the way you document that a client participated in and completed a session with you Depending on the billing process you have, a completed therapy note may also be the way a claim is generated Documentation also demonstrates your competency and shows how a client's needs have been addressedS – The S stands for Scripture you physically write out the scriptureyou'll be amazed that what God will reveal to you just by taking the time to slow down and actually write out what you are reading!Today, the SOAP note – an acronym for Subjective, Objective, Assessment and Plan – is the most common method of documentation used by providers to input notes into patients' medical records They allow providers to record and share information in a universal, systematic and easy to read format Opening a new medical practice?



Ppt Nutritional Progress Notes Powerpoint Presentation Free Download Id
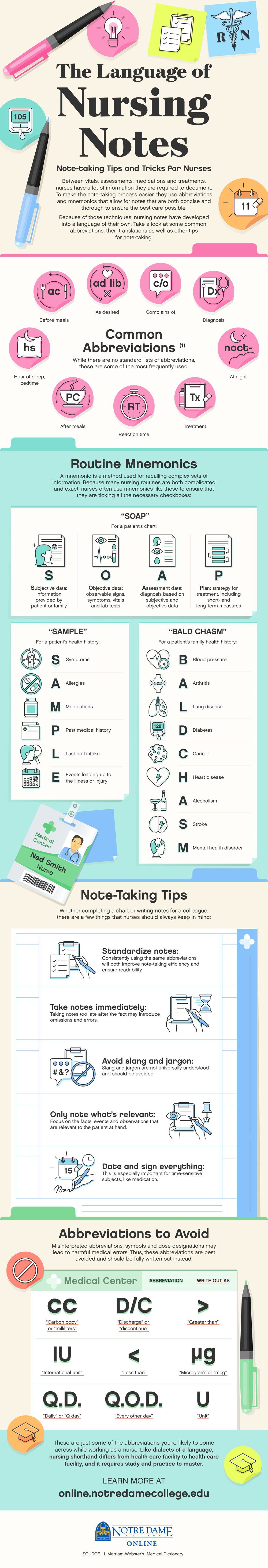



The Language Of Nursing Notes Mnemonics Notre Dame College Online
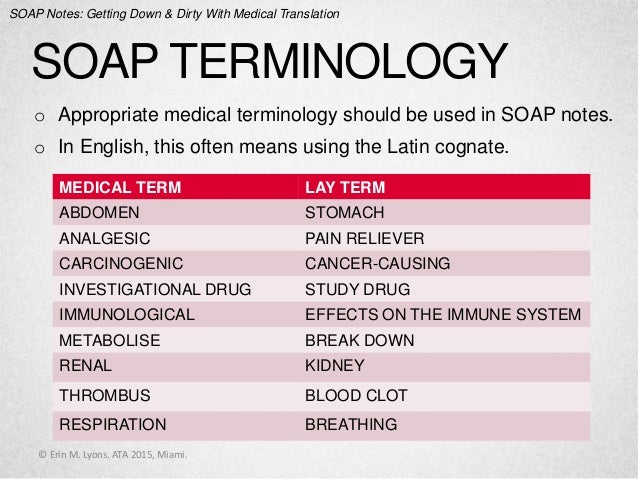
1Client words 2 Clarity 3 Completeness 4 Concise 5 Chronological order 6 Confidentiality This is a good technique for keeping for notes short and sweet, but to the point and with the accurate information Nurses can use this techniques as well SOAP notes, though, is a documenting format that is used to get the nursing process on the way Most practitioners who implement the use of SOAP notes report that it improves workflow, and often, patient outcomes Having a set method for reviewing the notes from a patient's last visit makes the next visit quicker Also, using a set format may allow the DC to see patterns more easily and clearlySOAP subjective, objective assessment plan SOB shortness of breath S/P, s/p status post (previous condition) sp cd spinal cord spec specimen sp fl spinal fluid sp&H speech and hearing spin spine, spinal spont spontaneous s/s signs and symptoms SS social service ST speech therapy stat, STAT immediately STD sexually transmitted disease



Help With Soap Note Development By Jasem James Fiverr




Soap Note Writing
40 Fantastic SOAP Note Examples & Templates If you have worked or are currently working in a hospital, you probably already know what a SOAP note is If not, let's learn all about it SOAP notes are written documentation made during the course of treatment of a patient A SOAP note template comes in a very structured format though it is only The term chiropractic "SOAP notes" has nothing to do with working up a lather So what does "SOAP" stand for?Start studying HOPS and SOAP definitions Learn vocabulary, terms, and more with flashcards, games, and other study tools




51 Sample Soap Notes In Pdf Ms Word Excel



Understanding Clinical Notes This Article By Dot Health Medium
SOAPIE An acronym for a charting mnemonic S ubjective, O bjective, A ssessment, P lan, I mplementation, E valuationSometimes they simply state in a narrative way the same informationTaken from Massage Therapy, Principles and Practice, 3rd edition by Susan Salvo Learn with flashcards, games, and more — for free




The Evolution Of Office Notes And The Emr The Caps Note Consult Qd




Transitioning To Soap 2 0 Webpt Emr Help
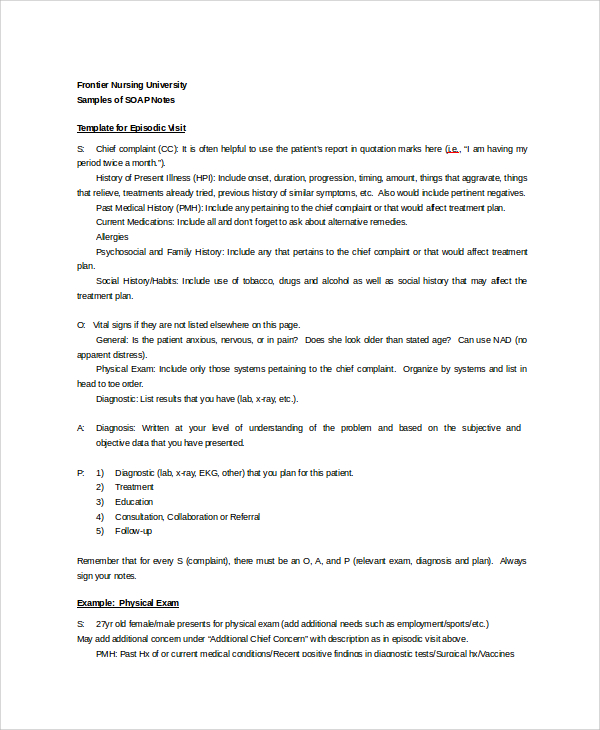
The SOAP note is considered a legal document, it can be used for third parties (medicare, insurance etc) protects the massage therapist if the patient have any concerns regarding their care reinforce massage treatment progress used for referral and communication purposes with the patient's other health care providers SOAP Notes Dentistry Example 1 Chief Complaint 23 year old male presents w/ a chief complaint of "my lower left back jaw has been sore for the past few days"S History of Present Illness Pt relates history of swelling for past 3 days, asymptomatic previously Medical History Med Conditions Medications Allergies Past Sx Social Hx Asthma Albuterol None Ear Lac 09 The notes you take as a behavioral health care professional determine the quality of care your patients receive Having notes that are comprehensive yet concise, and informative yet easy for other professionals to use is a skill that often takes years to master



Progress Notes



Physical Therapy Soap Note Example Therapy Daily Note
When confronted with a reading passage or document, students need a process to help them begin to determine the purpose or significance of the document It will then be much easier to interpret or even gather evidence from the document when students have a literacy tool to help them The acronym SOAP stands for Subjective, Objective, Assessment, and Plan Each category is described below S = Subjective or symptoms and reflects the history and interval history of the condition The patient's presenting complaints should be described in some detail in the notes of each and every office visitA SOAP note is a document usually used in the medical fraternity to capture a patient's details in the process of treatment This is one of the many formats that



Physical Therapy Soap Note Example Therapy Daily Note




Jm Rom Anatomical Terms Of Motion Musculoskeletal System
Symbolic Optimal Assembly Program (programming language for the IBM 650 computer in the late 1950's) SOAP Spectrometric Oil Analysis Program SOAP Small Operator Assistance Program SOAP Satellite Orbit Analysis Program (standard programO – The O stands for observation what do you see in the verses that you're reading? (Source) A SOAP (s ubjective, o bjective, a ssessment, p lan) note is a method of documentation used specifically by healthcare providers SOAP notes are used so staff can write down critical information concerning a patient in a clear, organized, and quick way



Soap Notes Getting Down And Dirty With Medical Translation




Dap Notes
Why use SOAPS when interpreting Primary Source documents?SOAP acronym for subjective data, objective data, assessment, plan, the way the progress notes are organized in problemoriented record keeping soap sōp any compound of one or more fatty acids, or their equivalents, with an alkali Soap is detergent and used as a cleanser green soap (medicinal soap) (soft soap) a soap made from vegetable oils otherSOAP A chart note usually follows a very simple pattern Subjective (what the patient thinks) = S Objective (what the doctor thinks) = O Assessment (what the diagnosis is) = A Plan (what happens next) = P Not all providers dictate the "SOAP" note format;



Http Dns3 Estudiocom Com Br Download Examples Of Nursing Notes Documentation Pdf




What Is A Soap Note Jess Brantner Wvu Dietetic Intern
The SOAP Acronym SOAP is an acronym for the 4 sections, or headings, that each progress note contains Subjective Where a client's subjective experiences, feelings, or perspectives are recorded harm come to a client's reputation Be sure to keep SOAP notes secure and accessible only to staff who work directly with the client SIDEBAR SOAP Note Example Here is an example of a SOAP note for a client who has type 2 diabetes Date 2/15/08 Subjective Client said, "I am happy now that I have gone down a pants size" FeelingA SOAP note is a documentation format that massage therapists and other healthcare workers use to document client encounters SOAP is an acronym that stands for subjective, objective, assessment and plan In this post, I'll discuss what information goes in




Soap Notes The St John S Pa Program Survival Guide




Web Service Wikipedia
IBM defines an SOP simply as "a set of instructions that describes all the relevant steps and activities of a process or procedure" It's crucial that organizations know what is needed to complete certain tasks or processes, and an SOP offers that guidance An SOP lays out the tasks and roles needed to achieve a policy outcomeWhat does SOAP mean? What Does SOAP Stand For?



Tips For Writing Better Mental Health Soap Notes Updated 21



1
Writing great Physical Therapist SOAP notes is a tried and true method for collecting data This data provides reference points throughout a patient's journey that can help you and your colleagues treat future patients with better accuracy 3 Information Sharing Among PeersS O A P NOTE = Subjective or summary statement by the client Usually, this is a direct quote The statement chosen should capture the theme of the session If adding your own explanatory information, place within brackets to make it clear that it is not a direct quoteWriting progress notes SOAPE style SOAPE Subjective The story so far main problems, presumptive diagnosis, tests and treatments;
.png)



Free Massage Soap Notes Forms Massagebook



How To Write A Soap Note Occupational Therapy
Who is the audience?There are four components that form these notes that make up the acronym SOAP S is for subjective, or what the patients say about their situation ItIt stands for "Subjective Objective Assessment Plan," which provides documentation of a patient's condition, diagnosis and treatment SOAP notes were invented in the 1960s by Dr Lawrence Weed of the University of Vermont




Soap Note Templates Safetyculture



Www Ashp Org Media Store Files P2449 Sample Chapter 6
The Subjective section of your soap note is about what the patient is experiencing and how they are handling their concerns Some common examples may include chest pain, decreased appetite, and shortness of breath You can also talk to a family member or spouse to get any necessary information Using SOAP is good medicine Michael H Riegger, DVM, DABVP We all see these articles about what it takes to run a successful practice slick marketing, conflict management, Web pages, team training, appropriate compensation packages, etc The list is endless "You get the best out of others when you give the best of yourself"




4 Common Mistakes To Avoid When Writing Soap Notes Simplepractice




Transitioning To Soap 2 0 Webpt Emr Help



Nutritional Progress Notes Ppt Video Online Download



Dietetics Nutritioncare Clinical Documentation 18 Ubc Wiki




How To Write Incredible Physical Therapist Soap Notes



Patient Soap Note Charting Procedures



How To Take Clinical Notes Using Da R P



40 Fantastic Soap Note Examples Templates ᐅ Templatelab




Medical Terminology And Abbrev Pages 1 10 Flip Pdf Download Fliphtml5




Client Intake Forms Agreements Acuity Scheduling




Soap Note Dental Hygiene School Medical Assistant Classes Dental Assistant Study




How To Write A Soap Note Writing Guide A Research Guide For Students




Free Soap Notes Templates For Busy Healthcare Professionals



What Are Soap Notes In Counseling Examples



Http Www Drkney Com Videos k 11 Basic Progressnote Pdf




What Are Soap Notes In Counseling Examples



Counseling Soap Note Example Studocu
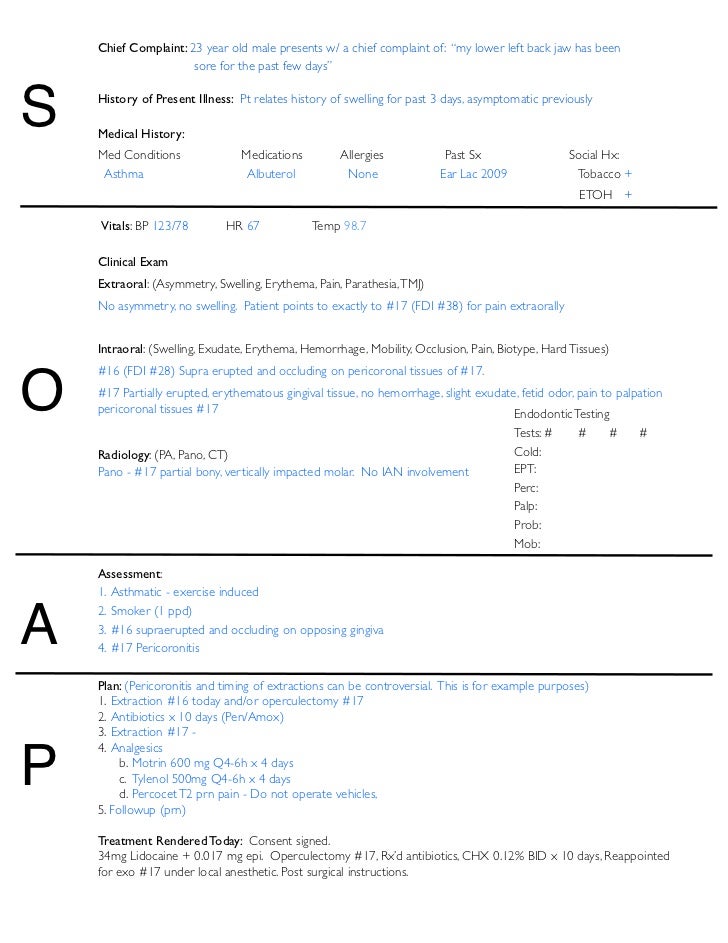



Soap Notes Dentistry Example




Chiropractic Travel Card




Soap Note How To Write Spotless Healthcare Notes Free Template Process Street Checklist Workflow And Sop Software



Soap Note How To Write Spotless Healthcare Notes Free Template Process Street Checklist Workflow And Sop Software




Soap Note How To Write Spotless Healthcare Notes Free Template Process Street Checklist Workflow And Sop Software
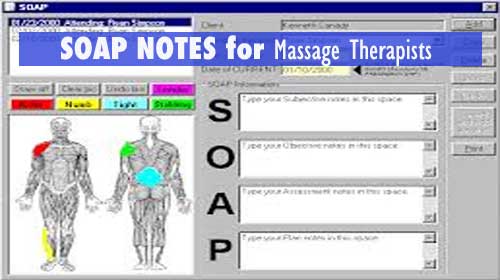



Soap Notes For Massage Therapy




Documentation And Coding Practices For Risk Adjustment And Hierarchical Condition Categories




Soap Note




Writing Soap Notes Step By Step Examples Templates




Examples Of Soap Notes In Nursing Video Lesson Transcript Study Com



Wilderness Medicine Training Center S Blog
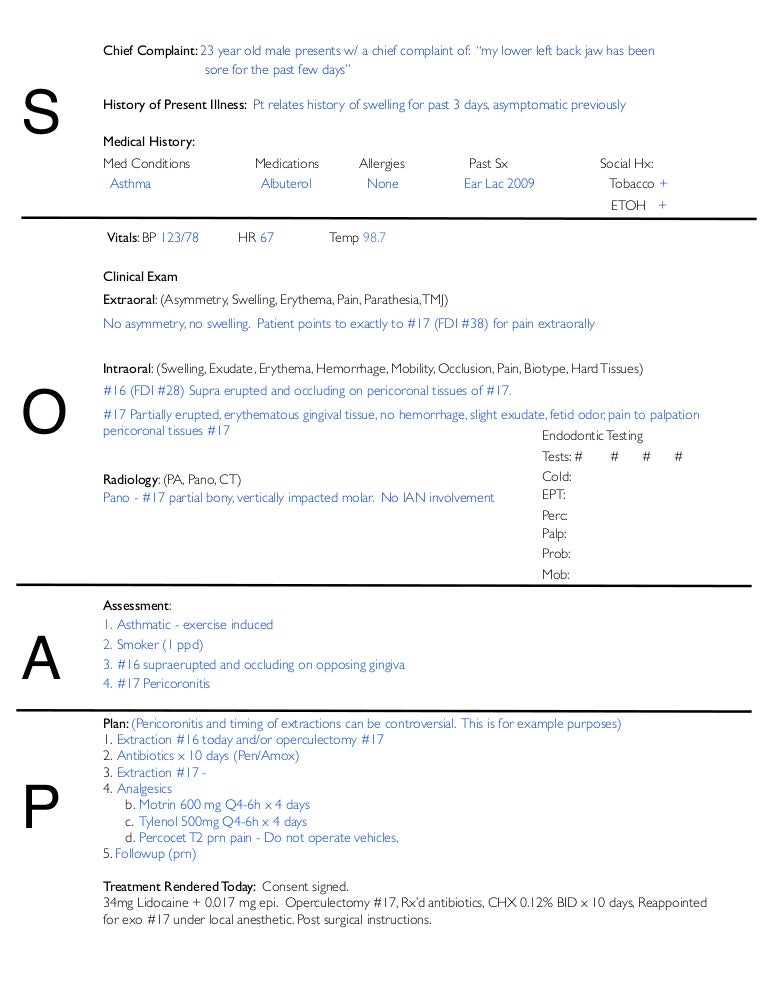



Soap Notes Dentistry Example




The Evolution Of Office Notes And The Emr The Caps Note Consult Qd



40 Fantastic Soap Note Examples Templates ᐅ Templatelab



Soap Note Guide Youtube




How To Write Massage Therapy Soap Notes Mblexguide



Tips For Writing Better Mental Health Soap Notes Updated 21



Free Easy To Use Massage Therapy Soap Notes Massagebook Massagebook




Soap Note How To Write Spotless Healthcare Notes Free Template Process Street Checklist Workflow And Sop Software



The Language Of Nursing Notes Mnemonics Notre Dame College Online




Writing Soap Notes Step By Step Examples Templates




How To Write A Soap Note With Pictures Wikihow




Soap Note Flashcards Quizlet




Pdf Clinical Note Taking Is Very Challenging For Many Students That Are Novice In The Field Many Times Even Professionals Ask What Type Of Note Taking Is Easy For You So I




How To Write Incredible Physical Therapist Soap Notes




What Are Psychotherapy Notes Vs Progress Notes Theranest




What Are Soap Notes In Counseling Examples




4 Common Mistakes To Avoid When Writing Soap Notes Simplepractice



Health Science Self Guided Soap Notes Exploration By Laura Miller




Soap Notes Resources Digital Chalkboard




Soap Wikipedia



How To Document A Patient Assessment Soap Geeky Medics




Note Templates In This Soap Note And Progress Note Kit Available For Therapy Notes Clinical Social Work Treatment Plan Template




Free Soap Notes Templates For Busy Healthcare Professionals




How To Improve Your Speech Therapy Soap Notes Power Diary



1
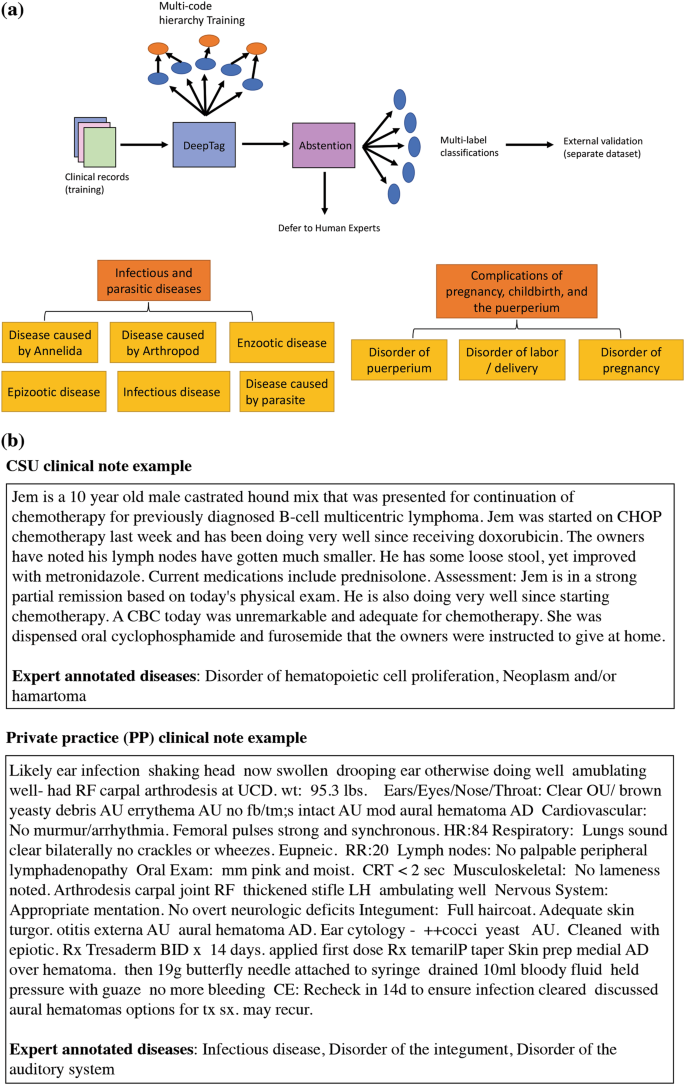



Deeptag Inferring Diagnoses From Veterinary Clinical Notes Npj Digital Medicine



1




Free Soap Notes Templates For Busy Healthcare Professionals



Soap Note Writing Tips For Mental Health Counselors Youtube




Rop Sports Medicine Lecture 5 S O A P Notes Ppt Video Online Download




Write A Soap Note How To Write A Soap Note




Soap Notes Flashcards Quizlet




Soap Notes Youtube



Free 18 Progress Note Examples Samples In Pdf Doc Examples




Understanding Soap Format For Clinical Rounds Global Pre Meds
%20for%20veterinary%20practices.jpg)



Soap Format Of Electronic Health Records Emrs For Veterinary Practices



Free 15 Soap Note Templates In Pdf Ms Word




How Soap Notes Paved Way For Modern Medical Documentation




College Certificate Programs Certificateprograms Occupational Therapy Quotes Soap Note Occupational Therapy Activities




How To Write Massage Therapy Soap Notes Mblexguide



Soap Note And Documentation Templates Examples Seniors Flourish




Birp Notes A Complete Guide On The Birp Note Taking Format



1



Www Nbome Org Docs Peorientationguide Pdf



Fcm Unm Edu Education Images Docs Template Clin Soap Note Pdf




Free Easy To Use Massage Therapy Soap Notes Massagebook Massagebook




Tips For Writing Better Mental Health Soap Notes Updated 21




Social Workers Easy Way To Write Soap Notes Youtube




What Is Soap Notes How Standardized Notes Improve Healthcare 5 Holland Irvine Ca Usa Cybernet Asia Cybernet Europe Cybernet Usa
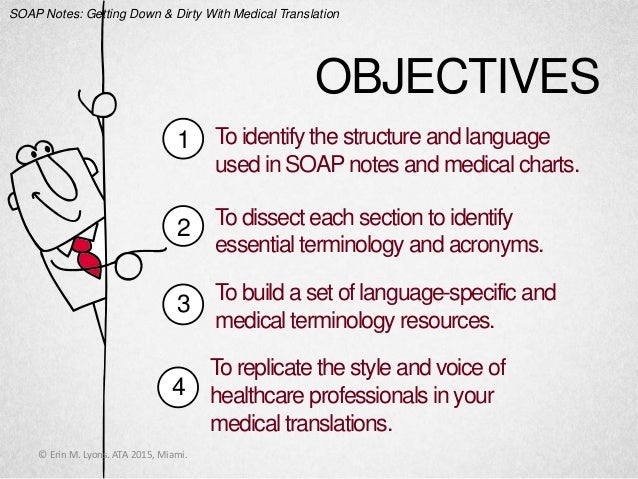



Soap Notes Getting Down And Dirty With Medical Translation



0 件のコメント:
コメントを投稿